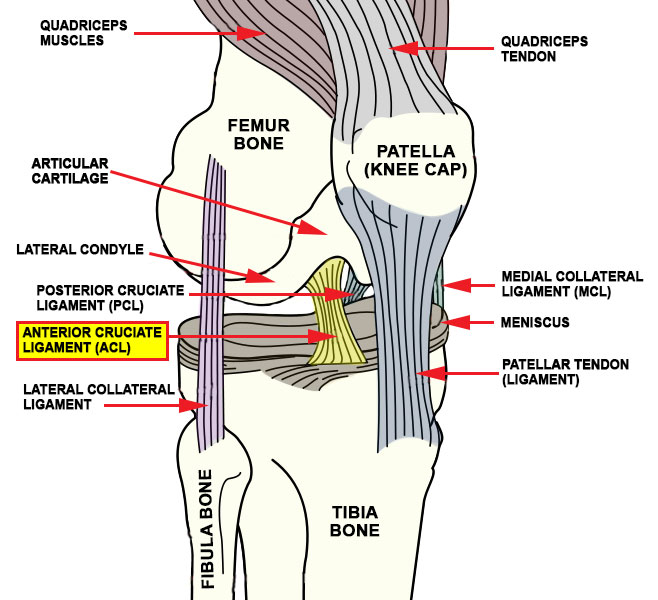
Denver MCL Specialists Diagnose MCL Injuries to Keep Coloradans Active

Denver MCL specialists continue to see a high volume of MCL injuries. The medial collateral ligament (MCL for short) is in fact the most frequently injured ligament of the knee – accounting for as many as 40% of knee ligament injuries. And because minor MCL injuries often go undiagnosed, this number is likely low. But […]
Non-surgical treatments for knee arthritis
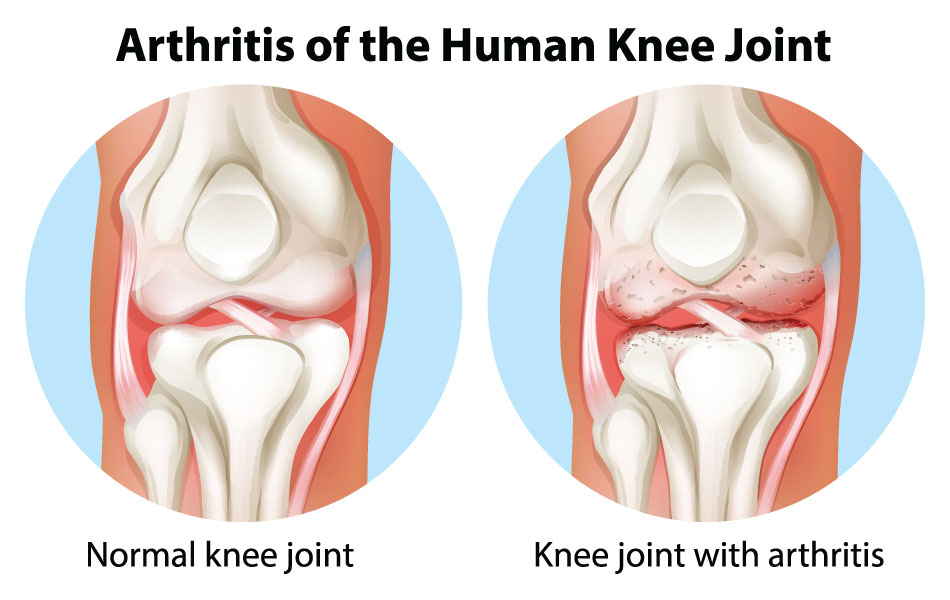
As we outlined in our first knee arthritis post in this three-part series, there is no cure for knee arthritis, so beware of ‘miracle cures’ that claim otherwise. If you have knee pain and think it might be knee arthritis, getting treatment can still reduce pain and minimize or delay long-term damage. There are many […]
Will it snow soon? Why your knee arthritis lets you know and how it impacts your joints.

Did you know that in the past 60 years, it has snowed on either Halloween or November 1st a whopping 41 times? While it looks like we’ll buck the trend this year with forecasts in the 70s for both days, winter is still coming! Maybe you can even feel it. Are you one of those people […]
Knee Arthritis
[av_textblock size=” font_color=” color=” custom_class=”] Causes | Treatment | Surgery [/av_textblock] [av_textblock size=” font_color=” color=” custom_class=”] Arthritis is inflammation in the joints or area of the body where two bones come together. Joints are responsible for the movement of body parts. It is a condition that can be experienced all over the body or in a […]
Collateral Ligament Injuries
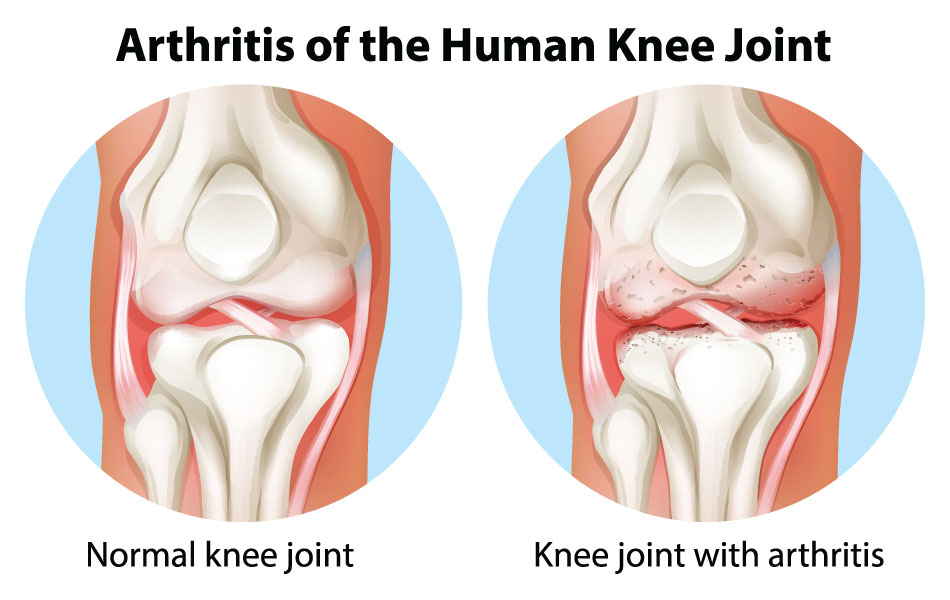
Meniscal Tear
[av_textblock size=” font_color=” color=”] Signs & Symptoms | Causes | Diagnosis | Prevention | Treatment | Conservative | Surgery | Rehabilitation [/av_textblock] [av_textblock size=” font_color=” color=”] A meniscal tear is a rupturing of one or more of the fibrocartilage strips in the knee called menisci. When doctors and patients refer to “torn cartilage” in the knee, they actually may be […]
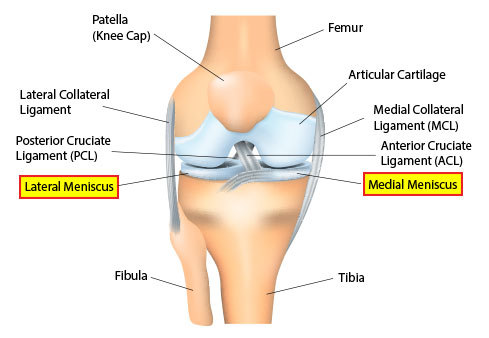
Anterior Cruciate Ligament (ACL) Injuries
[av_textblock size=” font_color=” color=”] Signs & Symptoms | Causes | Diagnosis | Prevention | Treatment | Conservative | Surgery | Rehabilitation [/av_textblock] [av_one_full first min_height=” vertical_alignment=” space=” custom_margin=” margin=’0px’ padding=’0px’ border=” border_color=” radius=’0px’ background_color=” src=” background_position=’top left’ background_repeat=’no-repeat’ animation=”] [av_textblock size=” font_color=” color=”] The anterior cruciate ligament (ACL) is an important internal stabilizer of the knee joint, restraining hyperextension. Anterior cruciate […]
Do you miss your meniscus? Q&A with Dr.Wayne Gersoff

At Advanced Orthopedics, we know that active lifestyles are a way of life in Colorado, and knee pain shouldn’t get in the way of your day-to-day activities or your fitness. There are multiple causes of knee pain and today we’ll answer 3 questions about one commonly damaged area: meniscus cartilage. What are the menisci? They […]
Does your golf buddy have the solution to your knee or hip pain?

Knee or hip pain can be excruciating and when you are in pain, you want relief – pure and simple. And there is no shortage of advice on how to fix your joint problem, right? If your pain is keeping you from being active, you’ve probably had plenty of advice from well-meaning friends, fellow sports […]

