The Anterior Approach to Hip Surgery
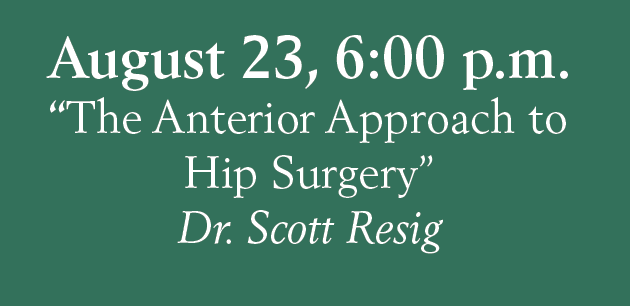
Seminar on August 23 at 6:30 pm at Sky Ridge Medical Center in the Auditorium on the Garden Level.
When is it time to consider shoulder replacement surgery?

And what type of surgery is right for you? Shoulder replacement surgery requires careful thought and planning, but for those who’ve exhausted other treatment options, it can be the best way to restore range of motion, relieve pain and help you return to an active lifestyle. Many different conditions can lead to the severe pain […]
Dr. Keith Jacobson Elected as 2018-2019 President-Elect by the American Board of Foot and Ankle Surgery

DENVER – July 26, 2018 –Advanced Orthopedic and Sports Medicine Specialists is pleased to announce that Keith Jacobson, DPM will serve as an executive officer of the 2018-2019 American Board of Foot and Ankle Surgery (ABFAS) President-Elect. His term begins September 1. Dr. Jacobson is board certified in reconstructive rear foot/ankle surgery and foot surgery […]
Painful bump on the side of your big toe? Why you shouldn’t ignore a bunion.

That painful bony bump on the side of your big toe? It’s probably a bunion. Nearly a quarter of people age 18-65 have bunions, making them one of the most common foot issues among adults. They also run in families and are more prevalent among women (thanks, cute heels), and among those over 65. In […]
Orthopedic Centers of Colorado Selects Clarify Health as Partner for Real-Time Patient Guidance
Colorado’s largest independent orthopedic, spine, and hand surgery group deploys Clarify’s Care Journey Platform to streamline clinician workflow and improve patient experience June 19, 2018 08:00 AM Eastern Daylight Time READ MORE>>

