Non-surgical treatments for knee arthritis
As we outlined in our first knee arthritis post in this three-part series, there is no cure for knee arthritis, so beware of ‘miracle cures’ that claim otherwise. If you have knee pain and think it might be knee arthritis, getting treatment can still reduce pain and minimize or delay long-term damage. There are many […]
Will it snow soon? Why your knee arthritis lets you know and how it impacts your joints.

Did you know that in the past 60 years, it has snowed on either Halloween or November 1st a whopping 41 times? While it looks like we’ll buck the trend this year with forecasts in the 70s for both days, winter is still coming! Maybe you can even feel it. Are you one of those people […]
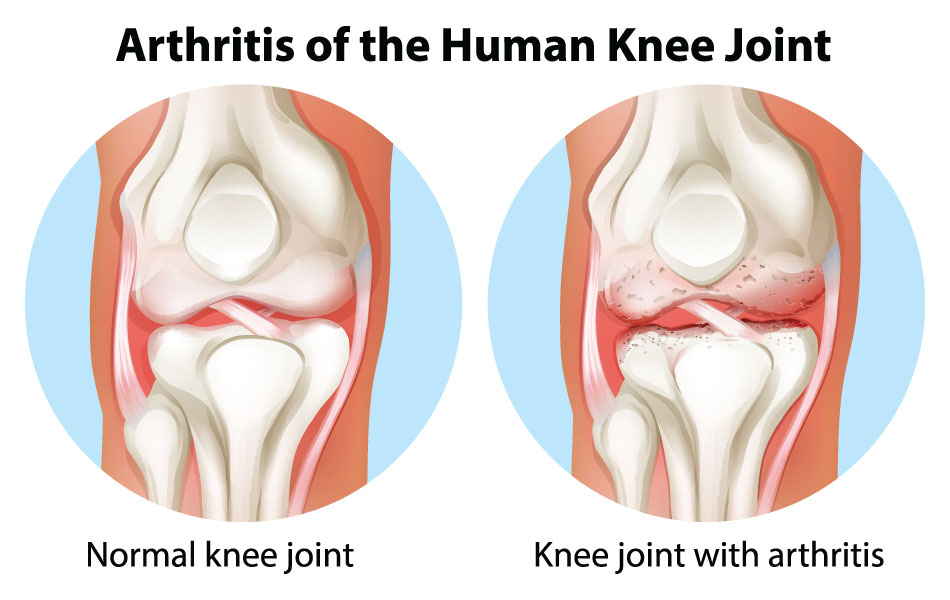
Knee Arthritis
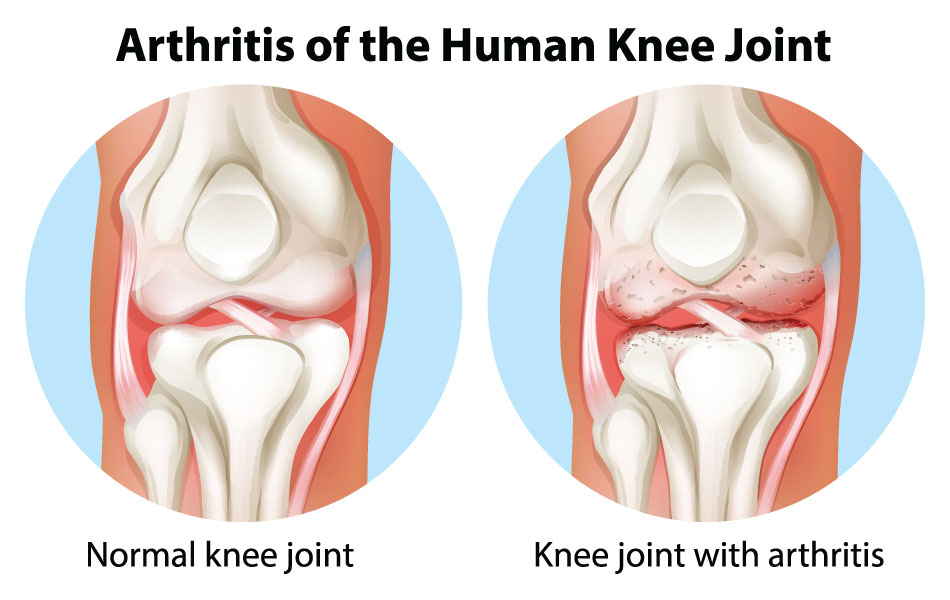
[av_textblock size=” font_color=” color=” custom_class=”] Causes | Treatment | Surgery [/av_textblock] [av_textblock size=” font_color=” color=” custom_class=”] Arthritis is inflammation in the joints or area of the body where two bones come together. Joints are responsible for the movement of body parts. It is a condition that can be experienced all over the body or in a […]
Not just an athlete’s problem: rotator cuff tears are more common than you think

Although also a common injury among athletes, rotator cuff tears are actually most common in people over 40; and age, in addition to family history and repetitive motion activities, are the top risk factors for a rotator cuff tear. The injury is also a frequent topic of discussion with baseball and tennis players, who […]

